02.01.02. The private health sector |
02.01.02. The private health sector |
02 Mar 2022
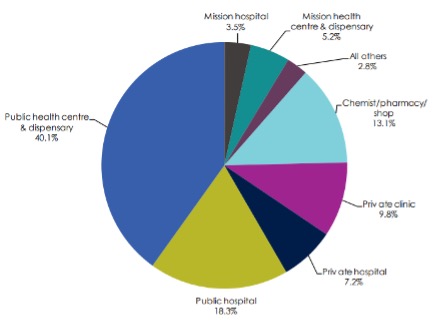
The percentage of individuals accessing private clinics and hospitals for outpatient services in general was 17% compared to over 58% in public facilities in 2013 (figure 1). However, there is a slightly higher dependence of private facilities in urban areas compared to rural areas (Ministry of Health, 2014a). Public outpatient visits was prevalent (66.7%) in rural areas followed by private health facilities visits (23.5%), whereas in urban areas, the visits were nearly equally distributed in both public (44.1%) and private (43%) health facilities (Ministry of Health, 2014a).
The quality of care provided in the privately owned facilities (visited by the middle or high socio-economic status individuals) is better in terms of drug availability and services provided including client focus and responsiveness, compared to that provided in public facilities or unlicenced private care facilities (used by the lower socio-economic statius individuals) (Berendes, Heywood, Oliver, & Garner, 2011). The huge disparities in health care service utilization is mainly due to differences in living standards, levels of education, household characteristics and expenditure (Ilinca et al., 2019).
Figure 1: Proportion of individuals accessing outpatient health services, 2013
The private sector is the largest employer of healthcare professionals in Kenya and has a private healthcare market of KES 20.7b (Barnes et al., 2010). The specific health care providers include informal health care providers such as traditional healers and faith healers; and Formal health care providers (disease-specific specialists, medical doctors, clinical officers and nurses) (Barnes et al., 2010).
Private health facilities are distributed all over the country with majority being medical clinics (2098), dispensaries (196) and nursing homes (150) (Ministry of Health, 2012).
References:
Barnes, J., O’Hanlon, B., Feeley, F., McKeon, K., Gitonga, N., & Decker, C. (2010). Private Health Sector Assessment in Kenya. 193(1). Washington, D.C. https://openknowledge.worldbank.org/bitstream/handle/10986/5932/552020PUB0Heal10Box349442B01PUBLIC1.pdf?sequence=1&isAllowed=y
Berendes, S., Heywood, P., Oliver, S., & Garner, P. (2011). Quality of private and public ambulatory health care in low and middle income countries: systematic review of comparative studies. PLoS Medicine, 8(4). https://doi.org/10.1371/journal.pmed.1000433
Ilinca, S., Di Giorgio, L., Salari, P., & Chuma, J. (2019). Socio-economic inequality and inequity in use of health care services in Kenya: evidence from the fourth Kenya household health expenditure and utilization survey. International Journal for Equity in Health, 18(1), 196. https://doi.org/10.1186/s12939-019-1106-z
Ministry of Health. (2012). Transforming Health: Accelerating attainment of Universal Health Coverage. The Kenya Health Sector Strategic and Investment Plan (KHSSP), (July 2014), 100. http://e-cavi.com/wp-content/uploads/2014/11/kenya-health-sector-strategic-investiment-plan-2013-to-2017.pdf
Ministry of Health. (2014a). 2013 Kenya Household Health Expenditure and Utilization Survey. Nairobi, Kenya. https://www.healthpolicyproject.com/pubs/745_KHHUESReportJanuary.pdf
